Cos’è l’Ipospadia
 L’ipospadia è una malformazione congenita dei genitali maschili principalmente caratterizzata da un incompleto sviluppo dell’uretra. Vi è un’anomala apertura dell’uretra, non all’apice del glande ma sulla superficie ventrale del pene. La pelle del pene (prepuzio) che normalmente ricopre il glande, è assente nella parte ventrale del pene ed esuberante nella parte dorsale. Questa anomala apertura dell’uretra può essere situata a qualunque livello, lungo il pene oppure nello scroto o nel perineo. L’ipospadia può associarsi ad una curvatura del pene (curvatura congenita) in erezione.
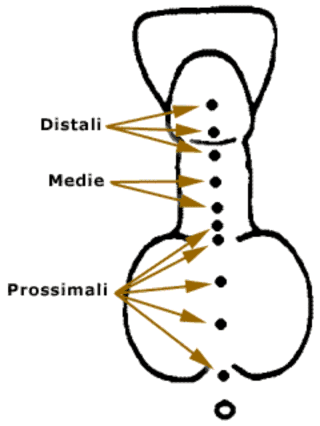
L’ipospadia è una malformazione congenita dei genitali maschili principalmente caratterizzata da un incompleto sviluppo dell’uretra. Vi è un’anomala apertura dell’uretra, non all’apice del glande ma sulla superficie ventrale del pene. La pelle del pene (prepuzio) che normalmente ricopre il glande, è assente nella parte ventrale del pene ed esuberante nella parte dorsale. Questa anomala apertura dell’uretra può essere situata a qualunque livello, lungo il pene oppure nello scroto o nel perineo. L’ipospadia può associarsi ad una curvatura del pene (curvatura congenita) in erezione.- glandulare – subcoronale (distali) 50% dei casi
- peniena (medie) 20% dei casi
- scroto-perineale (prossimali) 30% dei casi
Qual è l’incidenza dell’ipospadia e di anomalie associate?
L’ipospadia si presenta in circa lo 0.3% dei neonati maschi sani. Le anomalie del tratto urinario nei pazienti con ipospadia sono rare perché i genitali esterni si formano dopo l’alto apparato urinario. Il testicolo ritenuto e l’ernia inguinale costituiscono le condizioni patologiche più frequentemente (10% dei casi) associate all’ipospadia. Nelle forme di ipospadia scroto-perineale possono essere presenti complesse malformazioni ano-genitali e disordini cromosomici.
La diagnosi d’ipospadia può essere effettuata già in utero, durante la gravidanza, con esame ecografico del feto. La conferma diagnostica è comunque immediata al momento della nascita. I segni classici del pene con ipospadia sono la posizione anomala del meato uretrale e la presenza del tipico cappuccio di cute prepuziale sul dorso del pene.
Quale trattamento chirurgico per curare tale patologia?
Esistono principalmente 3 motivi che spingono all’intervento:
- Motivo funzionale:
il meato in posizione anomala impedisce di urinare in piedi.
Se il meato è ristretto non si riesce ad urinare con ripercussioni a livello vescicale e renale - Motivo sessuale:
l’eventuale presenza di una curvatura congenita del pene ostacolerà in futuro la penetrazione del pene in vagina.
L’anomala posizione del meato nelle forme gravi impedirà l’eiaculazione in vagina e quindi la capacità di fecondare la donna. - Motivo estetico:
l’ aspetto estetico del pene potrebbe causare importanti problemi psicologici.
L’intervento chirurgico vuole dare una risposta a tutti e tre i motivi funzionale, sessuale, estetico:
- portare il meato uretrale in cima al pene nella sua posizione naturale e ricostruire l’uretra mancante
- correggere la curvatura del pene
- creare un aspetto estetico simile alla normalità.
Il momento più opportuno per la correzione chirurgica dell’ipospadia è tra il 6° ed il 18° mese di vita, quando le conseguenze psicologiche di un intervento chirurgico sono minime.
La valutazione a lungo termine dei risultati nei pazienti sottoposti a chirurgia per ipospadia è difficile e spesso la valutazione del risultato da parte del chirurgo è differente rispetto a quella del paziente. Tutti i pazienti, quindi, dovrebbero essere seguiti durante l’adolescenza e dovrebbe essere offerta loro la possibilità di un’ulteriore correzione estetica se non sono soddisfatti. Comunque, con le attuali tecniche chirurgiche, il paziente nato con ipospadia ha un’elevata possibilità di avere una normale funzione sessuale, un normale mitto ed un’accettabile risultato estetico.
Complicanze dell’ipospadia
La chirurgia dell’ipospadia è caratterizzata dal 10-30 % di complicanze, soprattutto fistole e stenosi uretrali, che possono richiedere un ulteriore intervento chirurgico di riparazione a distanza di almeno 3 mesi dal primo.
Video Testimonianza Intervento a Belgrado
Intervento di Ipospadia Fallita
Video Testimonianza Intervento a Belgrado
Intervento di Ipospadia Fallita con Curvatura Ventrale










